Abstract
Introduction CAR-T therapy has resulted in durable complete responses previously unseen in treatment-refractory aggressive lymphoma. Immune effector cell-associated neurotoxicity syndrome (ICANS) is a well-described neuropsychiatric condition occurring frequently in the days to weeks after chimeric antigen receptor (CAR) T cell infusion. The syndrome is typically characterized by inattention, slowed response times, difficulty naming and disorientation. ICANS nearly always occurs after cytokine release syndrome (CRS) and usually resolves within 3-11 days. There is extremely limited data on long-term cognitive outcomes post-CAR T infusion. Our study seeks to characterize the long-term cognitive effects of CAR T therapy using detailed neurocognitive testing. Given the challenge of the COVID-19 pandemic, we evaluated the feasibility of in-person versus telehealth neuropsychiatric testing in all patients who received CAR-T treatment.
Study Design We conducted a pilot feasibility study of in-person versus remote neuropsychological testing for adults who were in remission at least 6 months after receiving axicabtagene ciloleucel (axi-cel) for large B cell lymphoma (LBCL). We sought to enroll 10 individuals in each study arms (in-person versus telehealth) identified through the Stanford CAR-T treatment database. The prospective cohort design was approved by our IRB and Scientific Review Committee. We set prespecified feasibility criteria as successful test completion in 7 of 10 subjects in each study arm.
Additional criteria included fluency in English and an ability to complete 90 minutes of in-person or telehealth neuropsychological testing independently. Exclusion criteria included enrollment in another clinical research study or active progressive lymphoma. Eligible study participants were randomly assigned to either in-person or telehealth neuropsychological testing, which was administered by trained psychometrists under the direction of a clinical neuropsychologist. Domains assessed were verbal memory, attention, processing speed and components of executive functioning that included fluency and set shifting. We also assessed quality of life (QOL) with the Short-Form 36 (SF-36) and screened for anxiety (GAD-7) and depression (PHQ-9).
Results We screened all patient with LBCL who received axi-cel been January 1, 2020 to January 31, 2022 and identify 33 patients who met study criteria. Via telephone screening, 19 patients consented to undergo neurocognitive battery testing (9 in-person and 10 telehealth). The remaining patients declined due to lack of interest, distance from Stanford, inaccessibility to Wi-Fi, unreliable transportation, or were not familiar with Zoom. These 19 subjects had an average age of 61.9 (range 28-75), 13 (68%) male, all had an ECOG of 0-1. All 19 subjects experienced CRS, (6 at grade 1 and 13 at Grade 2). 7 subjects experienced ICANS with 1, 2, and 4 experiencing Grade 1, 2, and 3 ICANS, respectively.
One subject failed to complete telehealth testing due to technical limitations. Nine participants were enrolled in the in-person testing arm and seven completed testing (one subject failed due to poor understanding of testing in English, one subject did not have transportation).
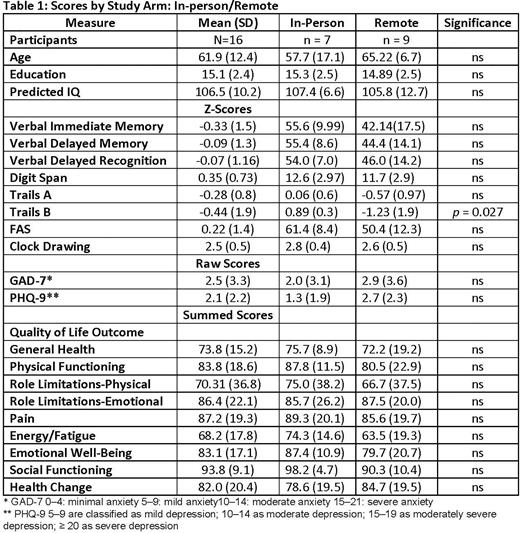
There was no difference between the remote versus in-person testing arms in terms of feasibility. Performance on neuropsychological tests and self-report of QOL and mood did not differ between groups, except for a set-shifting test, in which telehealth subjects performed lower. (Table 1) Five of 16 subjects (31%) performed below expected levels based on normative data from healthy controls. As a group, QOL and mood measures were within normal limits.
Conclusions/Future Directions We met our feasibility goals of at least seven subjects per testing arm, with 16 subjects successfully completing neuropsychological testing (84%) across the in-person and telehealth testing environments. Evidence of some cognitive impairment was seen in over 30% of participants. Baseline assessment in a larger cohort with neuropsychological testing at multiple time points longitudinally will allow for a more precise understanding of how CAR-T affects cognition, QOL and mood in individuals with prolonged recurrence-free survival.
Disclosures
Frank:Roche/Genentech - Wife: Current equity holder in private company, Current holder of stock options in a privately-held company; Kite/Gilead: Honoraria, Research Funding; Adaptive Biotechnologies: Consultancy, Honoraria, Research Funding; Allogene Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal